Achalasia Cardia is a condition that affects the esophagus, the tube that carries food from the mouth to the stomach. It occurs when the lower esophageal sphincter (LES) fails to open as it should during swallowing, leading to food backing up in the esophagus. One might wonder what causes achalasia cardia. It’s important to understand this as it can have a significant impact on everyday life due to difficulty in swallowing and associated pain. While not common, it does affect people around the world, with varying prevalence rates depending on the region.
The Esophagus and Achalasia: Digestion at a Standstill
The esophagus is a muscular tube that moves food from the throat to the stomach. Normally, as food reaches the end of the esophagus, the LES opens to let food enter the stomach. However, in the case of achalasia, this process doesn’t happen smoothly. Some reasons suggested for what causes achalasia cardia include nerve degeneration and autoimmune responses, where the immune system attacks the body’s own cells.
Recent research suggests that it could be linked to nerve cell damage in the esophagus. It’s also been thought that it’s related to immune system issues possibly triggered by a virus. Efforts to understand achalasia cardia vs gerd highlight the differences, as GERD involves the LES failing to close, causing acid reflux—a contrast to the failure to open in achalasia.
People with achalasia face serious disruptions in their digestive process. Food that doesn’t move to the stomach can cause discomfort and possible nutritional issues. Hence, recognizing what causes achalasia cardia is crucial as researchers continue to explore how exactly this disorder manifests.
Recognizing and Addressing Achalasia: Symptoms, Diagnosis, and Treatment
Recognizing achalasia cardia symptoms is the first step towards managing it. Common signs include:
- Difficulty swallowing food and drinks
- Chest pain after eating
- Regurgitating food
- Unexpected weight loss
Diagnosis involves simple tests. A barium swallow test is often used where a patient drinks a special liquid that shows up on X-rays, allowing doctors to see the esophagus’ shape and function. An esophageal manometry test measures the muscle pressure in the esophagus, helping doctors understand how well the esophagus moves food.
Lifestyle changes offer the first step in managing achalasia. Smaller, more frequent meals and avoiding eating before bed can help. An achalasia cardia diet that focuses on easy-to-swallow, soft foods minimizes pain and discomfort.
For more severe cases, medical treatments are essential. These include:
- Balloon dilation, where a balloon is used to widen the LES.
- Heller myotomy, a surgical procedure that cuts the muscle at the LES.
- POEM (Per Oral Endoscopic Myotomy), a less invasive surgery through the mouth to relieve pressure.
Surgery options for achalasia cardia offer relief but aren’t always necessary for everyone. Understanding these treatments helps patients make informed decisions.
Family history can play a role, as genetics often explain what causes achalasia cardia. If it runs in families, individuals may be at higher risk.
Dispelling Myths and Managing Achalasia: Diet and Community Support
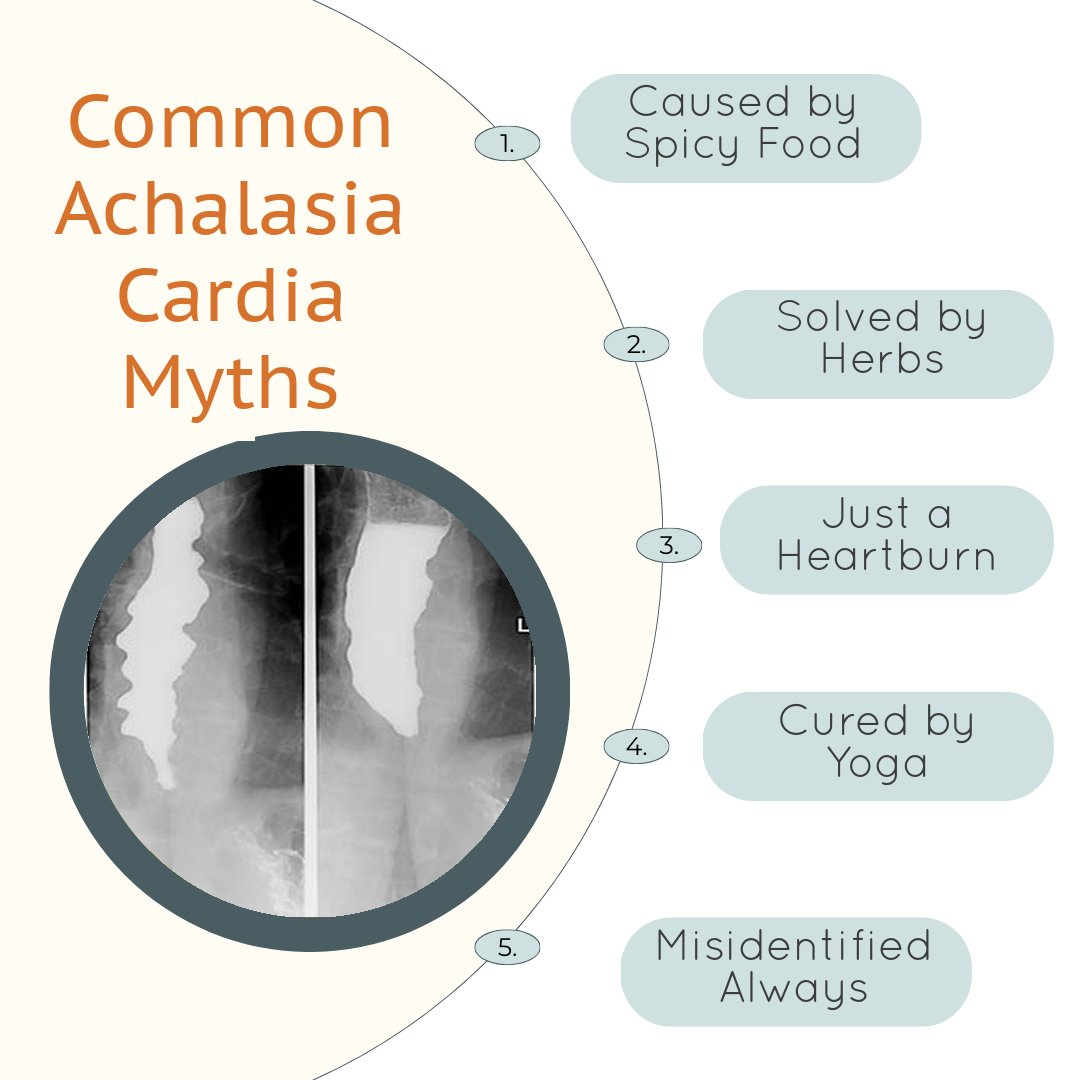
There are myths about achalasia, especially in different cultures such as India, where it might be confused with other digestive issues. Home remedies for achalasia cardia are sometimes believed to help, but professional medical advice is crucial.
For people with this condition, following a specific achalasia cardia diet is essential. Soft foods and plenty of fluids help in managing symptoms. Support networks can be invaluable. Engaging with community groups allows for shared experiences and practical advice.
Spreading knowledge about achalasia cardia symptoms and possible treatments helps build awareness. Encourage timely consultations with healthcare providers when symptoms arise.